In recent years, the term “black fungus” has gained significant attention due to its association with serious health complications. Scientifically referred to as mucormycosis, this fungal infection can be life-threatening if not detected and treated early. Understanding the black fungal symptoms, their early signs, and methods of prevention is crucial to protecting oneself and loved ones.
What Is Black Fungus (Mucormycosis)?
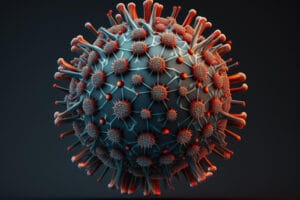
Black fungus, or mucormycosis, is a rare but severe fungal infection caused by a group of molds called mucormycetes. These molds are naturally present in the environment, especially in soil, decaying organic matter, and air. While these fungi are usually harmless to healthy individuals, they can cause severe infections in people with weakened immune systems or existing health conditions.
Who Is at Risk of Black Fungus?
Black fungus primarily affects individuals with compromised immune systems. This includes:
- Diabetes patients: High blood sugar levels create a favorable environment for fungal growth.
- COVID-19 survivors: The use of steroids and weakened immunity can increase susceptibility.
- Cancer patients: Chemotherapy and radiation therapy often impair immune defenses.
- Organ transplant recipients: Immunosuppressive drugs taken to prevent organ rejection make individuals more vulnerable.
- Individuals with prolonged steroid use or hospitalization: These factors can weaken the body’s ability to fight infections.
Understanding the risk factors is the first step toward identifying the black fungal symptoms and addressing them promptly.
Early Signs of Black Fungal Symptoms
Early detection of black fungus is important for effective treatment. Below are the common early signs and symptoms:
1. Facial Pain and Swelling

One of the most common black fungal symptoms is swelling or pain on one side of the face. This may start as a dull pain but can become intensive over time. The swelling often accompanies redness or tenderness. For instance, a patient recovering from COVID-19 might notice persistent facial discomfort, which should not be ignored.
2. Nasal Congestion or Black Discharge

The presence of blackish or brownish nasal discharge is a hallmark symptom. Nasal congestion that doesn’t improve with standard remedies can also indicate an underlying fungal infection. A real-world example is the case of individuals who initially dismiss these symptoms as sinus issues, only to later discover mucormycosis through medical tests.
3. Vision Problems

Black fungus can spread to the eyes, leading to blurred vision, double vision, or even vision loss in severe cases. The infection may also cause redness and swelling around the eyes. For instance, patients may find it difficult to focus or notice a shadow in their field of vision prompting an urgent need for medical evaluation.
4. Toothache or Jaw Pain

Patients often report unexplained toothache, jaw pain, or loosening of teeth. In advanced stages, the infection can damage the jawbone. A case study highlights a patient who underwent dental surgery, only to realize later that the symptoms were caused by black fungus.
5. Skin Lesions or Ulcers

If the infection spreads to the skin, it may cause blackened lesions, redness, or tender areas. These symptoms often develop in areas with prior injury or cuts. For example, a minor scratch that becomes unusually painful or discolored could be a sign of fungal infection.
6. Fever and Fatigue

A persistent fever accompanied by fatigue is another early indicator. While fever is a common symptom of many illnesses, it should not be ignored when combined with other black fungal symptoms. A patient recovering from an illness like COVID-19 might dismiss fatigue as normal, but when combined with other signs, it requires attention.
Advanced Symptoms to Watch For
If it is not treated, the infection can progress to more severe stages, causing symptoms such as:
- Severe headaches
- Mental confusion or altered consciousness
- Numbness or tingling in affected areas
- Difficulty breathing due to lung involvement
- Chest pain
These advanced symptoms are signs of a medical emergency and require immediate attention. For example, a patient who experiences both severe headaches and nasal discharge may be dealing with the spread of black fungus to the brain.
How to Prevent Black Fungus
Prevention is always better than cure, especially when it comes to life-threatening infections. Here are some effective ways to prevent black fungus:
1. Maintain Good Hygiene
Keeping your surroundings clean is important. Regularly wash your hands, avoid touching your face unnecessarily and clean household surfaces frequently. Good personal hygiene reduces the risk of fungal spores entering the body.
2. Manage Underlying Conditions
Managing chronic health conditions like diabetes is crucial. Keep your blood sugar levels under control and follow your doctor’s advice diligently. Poorly controlled diabetes is one of the leading contributors to black fungal symptoms. For instance, diabetic patients should monitor their glucose levels consistently and avoid negligence.
3. Avoid Prolonged Use of Steroids
While steroids are effective for treating certain conditions, prolonged use can weaken the immune system. Use steroids only under medical supervision and as prescribed. For example, during COVID-19 treatment, patients should be aware of the potential side effects of steroid overuse.
4. Wear Protective Gear
If you are working in environments with high exposure to dust, soil, or decaying matter, wear protective gear like masks and gloves. This precaution is particularly important for people with compromised immunity. For example, farmers or gardeners handling organic materials should use N95 masks.
5. Avoid Self-Medication
Taking antibiotics or antifungal medications without medical advice can disturb the body’s natural balance and make it more susceptible to infections. Always consult a professional doctor before starting any medication.
6. Monitor Post-COVID Recovery
COVID-19 survivors should stay vigilant during their recovery phase. Regular follow ups with your doctor can help notice any early black fungal symptoms, especially if steroids or oxygen therapy were part of the treatment.
Real-Life Example: Recognizing Black Fungal Symptoms Early
Consider the case of Ravi, a 45-year-old diabetic who recovered from COVID-19. A few weeks post-recovery, he began experiencing facial pain and nasal congestion. Initially, he dismissed these as minor issues but when he noticed black discharge from his nose, he consulted a doctor.
A nasal endoscopy revealed mucormycosis. Ravi’s early diagnosis allowed for prompt treatment with antifungal medication and surgery which saved his life. This case highlights the importance of identifying and acting upon black fungal symptoms early.
Similarly, another case involved a middle aged woman who developed blurred vision and toothache after COVID. Timely intervention and surgery prevented further complications and highlighted the importance of awareness and caution.
Treatment Options for Black Fungus
Treatment for black fungus involves a combination of antifungal medications and surgical intervention. Common treatments include:
- Antifungal Drugs: Amphotericin B is the most commonly used antifungal medication for treating mucormycosis. Patients often require intravenous administration over several weeks.
- Surgical Debridement: In severe cases, removing infected tissues through surgery may be necessary to prevent the spread of the fungus. For example: surgery may involve removing a portion of the jawbone or an affected eye in extreme cases.
- Addressing Underlying Conditions: Managing diabetes and other health issues is critical for recovery. For example, a diabetic patient undergoing treatment must work closely with endocrinologists to maintain stable glucose levels.
Early detection and immediate treatment significantly improve outcomes. Delayed intervention can lead to irreversible damage or even fatality.
When to See a Doctor
If you experience any of the symptoms mentioned above, especially after recovering from COVID-19 or while managing a chronic illness, consult a healthcare professional immediately. Delaying treatment will lead to severe complications including organ damage or even death.
For example: someone experiencing facial swelling combined with nasal discharge should not wait for symptoms to worsen before seeking medical advice.
Conclusion
Black fungus is a very serious condition that requires timely diagnosis and treatment. By understanding the early black fungal symptoms, recognizing the risk factors and adopting preventive measures, you can save yourself and your loved ones from this life-threatening condition.
Stay informed, practice good hygiene and seek medical help at the first sign of trouble. Awareness and care are your best tools to fight black fungus effectively.
Frequently Asked Questions
1. What are the early signs of black fungus?
The early signs of black fungus include facial pain or swelling, nasal congestion with black discharge, toothache, blurred vision, and skin lesions. Prompt medical attention is crucial for effective treatment.
2. Who is most at risk of developing black fungus?
Individuals with weakened immune systems, such as those with diabetes, cancer, or who have recovered from COVID-19, are at higher risk. Prolonged steroid use or organ transplants also increase susceptibility.
3. How can black fungus be prevented?
Prevention includes maintaining good hygiene, managing chronic conditions like diabetes, avoiding self-medication, wearing protective gear in high-risk environments, and regular medical follow-ups after recovering from illnesses.
4. What should I do if I notice black fungal symptoms?
If you experience symptoms like nasal discharge, facial swelling, or vision problems, consult a doctor immediately. Early diagnosis and treatment improve recovery outcomes significantly.
5. Can black fungus spread from person to person?
No, black fungus is not contagious and does not spread from person to person. It primarily occurs when fungal spores in the environment enter the body through the respiratory system or wounds.
Images By: FreePik




Pingback: Yellow Fungus Symptoms and How to Spot Them Early - Basaveshwar Hospital
Pingback: Black Fungus in Eyes Symptoms and Prevention